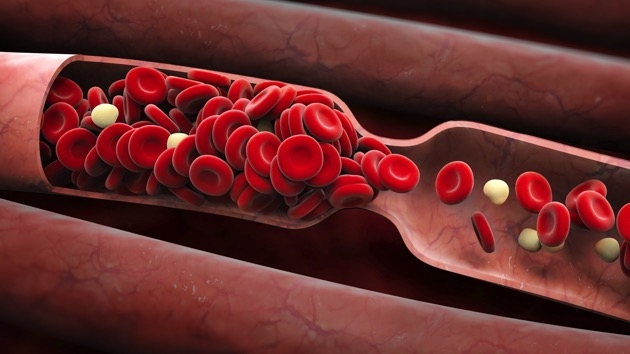
Blood clot, new deadly complication of COVID-19
 |
| (Photo: Connect FM) |
Apart from kidney issues and heart problems, doctors are also seeing blood clots in the lungs and bodies of patients. Clots can travel and create blockages in veins, leading to strokes, heart attacks, and other issues, Business insider reported.
Some of the patients with blood clots are in hospitals in critical condition, while others diagnosed with the COVID-19 complications are otherwise healthy enough to be sent home.
That's what happened to Michael Reagan, a 49-year-old COVID-19 patient.
'It feels like a toxin is in my body'
Reagan, who works for an international biomedical company in New York, was diagnosed with COVID-19 in late March and had been recovering at home in New York City for weeks. He was taking azithromycin, an antibiotic used to treat infections, and hydroxychloroquine, an antimalarial medication, as a participant in a clinical trial.
His COVID-19 symptoms included breathing problems, a high fever, and coughing up blood. Reagan said he was starting to feel a little better early last week until he suddenly began to experience a high fever once again, along with chest pains.
When he went into the hospital, Reagan said doctors told him coronavirus-related pneumonia had spread into both lungs. A pulmonologist later told him he had dozens of little blood clots throughout his lungs.
"It feels like a toxin is in my body," Reagan told Business Insider.
 |
Michael Reagan at Mount Sinai Hospital in New York for blood-clot treatment on April 14. (Photo courtesy of Michael Reagan) |
'Alarming' rates of blood clots
The Dutch study of 184 patients in the ICU with COVID-19-related pneumonia found that more than 20% were having clotting issues. A study of 81 similarly ill patients in Wuhan, China, found a 25% incidence of clots.
Dr. Behnood Bikdeli, who helped coordinate the international coalition of physicians looking into the clotting issue, called those numbers "alarming”, CNN reported.
In the three weeks beginning mid-March, Mocco saw 32 stroke patients with large blood blockages in the brain, double the usual number for that period.
Five were unusually young, under age 49, with no obvious risk factors for strokes, “which is crazy,” he said. “Very, very atypical.” The youngest was only 31.
At least half of the 32 patients would test positive for COVID-19, Mocco told Reuters.
Meanwhile, Dr. Hooman Poor, a Mount Sinai lung specialist, found himself working a late shift with 14 patients on ventilators. The ventilator readings were not what he expected.
The lungs did not seem stiff, as is common in pneumonia. Instead, it seemed blood was not circulating freely through the lungs to be aerated with each breath.
Poor ran into a kidney doctor that night, who remarked that dialysis catheters were often getting blocked with clots.
“And I said, ‘It’s funny that you mentioned that because I feel like all these patients have blood clots in their lungs,’” Poor recalled.
 |
Registered Nurse Arnold Garcia collects a sample for a coronavirus test from Michael Weiss after he was admitted with possible COVID-19 symptoms at Sharp Chula Vista Medical Center in Chula Vista, Calif., on April 10, 2020. (Photo: Stars and Stripes) |
Figuring out the best way to treat coronavirus complications
Blood clots can occur in severely ill patients in intensive-care units and even in patients who are hospitalized. While in the ICU, patients are typically on breathing support and sedated, which limits their ability to move as they heal. Staying still raises the risk of clots.
Some doctors think there's something about the coronavirus that leads to more clotting issues, though.
And in the absence of clinical trials and science-backed treatments, doctors are forced to figure out how to best treat these complications with relatively little guidance, Dr. Alex Spyropoulos, an expert on blood clots at Northwell Health in New York, told Business Insider.
As colleagues from various specialties pooled their observations, doctors developed a new treatment protocol. Patients now receive high doses of a blood-thinning drug even before any evidence of clotting appears, Reuters reported.
“Maybe, just maybe, if you prevent the clotting, you can make the disease less severe,” said Dr. David Reich, the hospital president. The new protocol will not be used on certain high-risk patients because blood thinners can lead to bleeding in the brain and other organs.
 | Coronavirus symptoms: 10 keys signs and how to protect yourself Any or all symptoms caused by the novel virus can appear anywhere from two to 14 days after exposure to the virus. Below are 10 ... |
 | Covid-19 patients could still be contagious 8 days after symptoms disappear Haft of the patients with mild COVID-19 infections in a study still carry the novel coronavirus 2.5 - 8 days after they’ve appeared to recover, ... |
 | Coronavirus symptoms: Sudden lost of smell and taste Evidence is growing that anyone experiencing a sudden loss of smell and taste could be a "hidden carrier" of the coronavirus, even if no other ... |
Recommended
 World
World
Pakistan NCRC report explores emerging child rights issues
 World
World
"India has right to defend herself against terror," says German Foreign Minister, endorses Op Sindoor
 World
World
‘We stand with India’: Japan, UAE back New Delhi over its global outreach against terror
 World
World
'Action Was Entirely Justifiable': Former US NSA John Bolton Backs India's Right After Pahalgam Attack
 World
World
US, China Conclude Trade Talks with Positive Outcome
 World
World
Nifty, Sensex jumped more than 2% in opening as India-Pakistan tensions ease
 World
World
Easing of US-China Tariffs: Markets React Positively, Experts Remain Cautious
 World
World







